Jonathan Riddle (Wheaton College) received his Ph.D. in history at the University of Notre Dame in 2019. Philip Byers recently caught up with Riddle to discuss his research on religion and pandemics.
Philip Byers: For several years, you were a South Bend resident and a regular presence around the Cushwa Center before moving in 2018. Catch us up on what the last two years have held for you professionally.

Jonathan Riddle: In 2018, while I was still writing my dissertation at the University of Notre Dame, Wheaton College posted a position in the history of Christianity in the United States. Given my training in this field and the importance of Wheaton College to the careers of scholars like my advisor, Mark Noll, I could not but apply. Fortunately, they took a chance on me.
During my first year, I did what most new faculty spend their days and nights doing: rushing to develop new courses! While it was sometimes hectic, I enjoyed this process. My classes afforded me the chance to jump headfirst into topics I care deeply about: the history of Christianity, the history of health and medicine, and the intersection of those two. I relished the chance to share the excitement of that inquiry with students. There was also the small matter of finishing my dissertation, which I defended in the spring of 2019.
The past year brought both greater stability and new challenges. As I began to settle into my courses, I also worked on an article that examines debates about the relationship between body and soul that accompanied the rise of physiology in the early 19th-century United States. Yet the coronavirus soon disrupted any sense of normalcy I was developing. The pandemic required that I switch to remote teaching, of course, but it also redirected my scholarly efforts. I have spent much of the quarantine reading and writing about religion amidst disease outbreaks.
I should say that I also regret the necessity of the Cushwa Center cancelling its Seminar in American Religion this spring. One of the joys of remaining in the Midwest has been continuing to learn from the community of scholars regularly gathered by the center.
PB: What first piqued your interest in the relationship between religion and medicine?
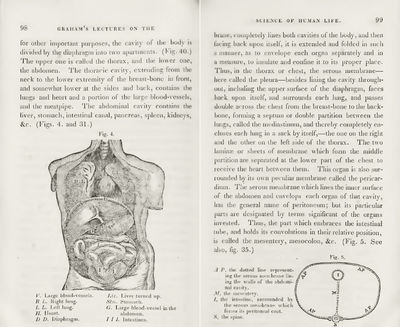
An excerpt from Sylvester Graham, Lectures on the Science
of Human Life, 2 vols. (Boston: Marsh, Capen, Lyon, and
Webb, 1839). Graham served as one of the foremost
leaders of the antebellum physiological reform movement.
JR: Some combination of curiosity and intuition led me to this field. I began my graduate training in the history of religion. But then I encountered some 19th-century sources discussing the spiritual importance of dietary choices. I had never read about health reform before, so I had lots of questions. Did 19th-century Americans not divide human nature the way we tend to, trusting the body to doctors and the soul to clergy? I had a sense, deriving from my reading in religious history and, perhaps, my own experience, that there was a story to be told here.
As I dug into the history of early 19th-century health reform, I discovered that both medical doctors and Protestant ministers helped lead this movement. They moved fluidly between their two domains, promising physical health and spiritual progress for Americans who diligently watched their diet. To tell this story, then, I needed expertise in the histories of both physiology and faith. So, in addition to Noll and the impressive array of religion scholars I was working with, I turned to Chris Hamlin and the History and Philosophy of Science Program at Notre Dame to help me understand the history of health and medicine.
Now that I have been working on religion and medicine for a few years, I am more convinced than ever of the need for historians to examine this relationship. In the past few weeks, for example, as people have looked for historical precedent to help them understand the current health crisis, many have wondered about religious responses to pandemics in the past. In some cases, there is good scholarship to guide them. In other cases, the history simply has not yet been written.
PB: Your dissertation addressed not only medicine and religion but also capitalism. To what degree are matters of faith and public health related to issues of wealth and poverty?
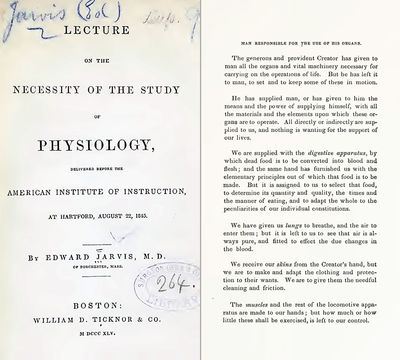
Pages from Edward Jarvis, Lecture on the Necessity of the
Study of Physiology (Boston: William D. Ticknor, 1845). The
prolific physician Edward Jarvis urged people to study
physiology as part of “man’s responsibility for his health.” As
Jarvis explained, “The generous and provident Creator has
given to man all the organs and vital machinery necessary
for carrying on the operations of life. But he has left it to
man, to set and to keep some of these in motion.”
JR: In my dissertation-turned-book project, I argue that physiology, liberal Protestantism, and marketplace capitalism combined to reinforce the touchstone principle of American healthcare: personal responsibility. Antebellum health reformers believed that physiology clearly illuminated the path toward robust health, that people had the moral agency and obligation to pursue that health, and that the result of their efforts would be individual and collective prosperity. While this gospel of personal responsibility offered a hopeful vision of self-improvement, it was inaccessible to many Americans. Health reformers worked from a place of privilege, preaching a universalizing yet individualistic gospel that reflected their status as white Protestants of the middling classes while ignoring the structural disparities of race, class, and gender that circumscribed Americans’ ability to control their own health.
In the following decades, personal responsibility continued to operate as a central ethic in American discussions of health. It continues to do so today. The notion is now shorn of overt Protestant theological reasoning, but it remains a moral mandate, one articulated in the language of epidemiological “risk factors” rather than spiritual obligation. It also continues to obscure the ways social location (to say nothing of genetics) governs just how much agency anyone wields in matters of health. Debates surrounding the coronavirus pandemic illustrate this dynamic well. As data began to reveal the stark racial disparities in covid-19 casualties, attention turned to the underlying conditions and comorbidities that rendered racialized minorities especially vulnerable to the disease. Some commentators responded by urging those communities to take responsibility for their health, whether by eating better or exercising more, and thereby reduce their risks. This advice sometimes ignored how structural and scientific racism, economic inequality, gender bias, citizenship status, incarceration, lack of health insurance, and other compounding factors have long undermined the health of marginalized communities in the United States. The notion of personal responsibility, nourished by deep religious roots, thus comports well with laissez-faire visions of the public sphere, but it fails to fully explain health disparities or motivate collective sacrifices to mitigate those disparities.
While personal responsibility has proven powerful in the history of health and medicine, it has not gone unchallenged. Critics, including people of faith, have interpreted the disproportionate physical suffering of marginalized people not as fitting punishment for poor decisions but as condemnation of the systems that marginalize. This approach has yielded everything from religious healthcare ministries to social justice activism in the name of Jesus. Today, for example, the Poor People’s Campaign has called for governmental responses to the coronavirus pandemic that meet the needs of vulnerable people now and address systemic injustices in the long term.
PB: You recently published at ChristianityToday.com a well-received piece on religion and the history of pandemics—tell us a bit about your experience of writing for a general audience. What are your ambitions in terms of doing public history, and how do you perceive the historian’s role in discussions about contemporary policy issues?
JR: I did not begin with grand ambitions. In early March, however, as the severity of the global health crisis became clear, friends encouraged me to write something for a popular publication. I regularly teach about the 19th-century cholera epidemics, so I turned to those crises as useful points of comparison for the present pandemic. I hoped making these comparisons would reveal some of the dynamics discussed above, as Christians responded to cholera epidemics in ways that reflected their convictions about moral responsibility for health. Overall, I enjoyed the process. Writing for a general audience felt quite similar to teaching. I will say, though, if I were to try to make a living through such work, I would need to learn to write more quickly!
As I see it, the task for historians of medicine during a pandemic is to take opportunities without being opportunistic. I cannot rejoice as I suppose many historians must when their happier topics hit the headlines. Rather, it is a time to grieve. So, if I am to engage the public, I must not do so in hopes of exploiting other people’s suffering for my own gain. At the same time, I believe historians of medicine do have something to contribute to our understanding of the pandemic and our discussions about how best to respond. The opportunity, then, is to respond in the spirit of service. I would prefer to think about the public historian’s role in terms of faithfulness to vocation rather than opportunism. What opportunities have I been given and therefore what responsibilities do I have?
PB: Where do you anticipate your scholarship heading next?
JR: After finishing my project on health reform, I plan to begin working on a religious history of 19th-century medicine more broadly. I will start by exploring the religious lives of healthcare professionals on either side of the slavery question, especially African American abolitionist doctors like John S. Rock.
Philip Byers worked at the Cushwa Center as a research associate in 2019–2020 while completing his doctorate in history at the University of Notre Dame. He has received a Mellon Fellowship to join the Cushwa Center in 2020–2021 as a postdoctoral research associate.